RECTAL CANCER IN A FEMALE PATIENT DISAPPEARED WITH COMBINED GENE THERAPY, CHEMOTHERAPY AND RADIATION
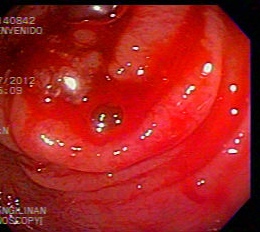
A 65 year old widow seen in the U.S. for bowel obstruction in September 2012. Findings were a pinpoint rectal opening. Biopsy showed invasive rectal adenocarcinoma. Abdomen and Pelvic CT scans showed thickening of the rectal wall as well as anus, consistent with rectal carcinoma, with obliteration of the fat pad within the rectum and vagina. Chest CT scan on the same day also showed no metastasis.
She decided to come to the Philippines for further treatment and underwent laparoscopic sigmoid colostomy.
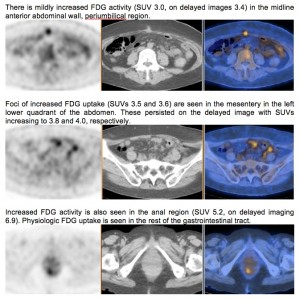
On October 2012 she underwent PET-CT scan. Findings showed hypermetabolic foci in the anterior abdominal wall and left lower quadrant of the abdomen (post surgical changes), and anal region.
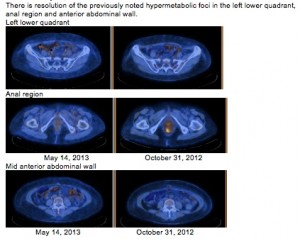
Beginning on November 2012, she underwent neoadjuvant chemotherapy every 2 weeks using Folfox. She also underwent twice weekly infusion of Gendicine for 12 times. She had external beam radiation therapy (EBRT) via intensity modulated radiation therapy (IMRT) to the pelvis from Feb to March 2013, with a total dose of 5,040 cGy given in 28 fractions. By the time she was evaluated for definitive surgery, she has completed 5 cycles of Folfox and 12 cycles of Gendicine and radiation. Another PET-CT scan was done in May 2013 which showed interval resolution of the hypermetabolic foci in the left lower quadrant of the abdomen, anal region and mid anterior abdominal wall.
On April 2013, an endorectal ultrasound was done by a gastroenterologist, which he interpreted as equivocal. No biopsy was thus done.
In May 2013, under general anesthesia a colorectal surgeon did bimanual examination, vaginoscopy, fine needle aspiration biopsy of the thickened anovaginal septum, Hegar dilatation of the anal stricture, proctoscopy, and endorectal ultrasound. His findings: no vaginal mucosal abnormality except for some congested mucosa at the distal posterior vaginal wall. Thickening of the anovaginal septum. Anal canal significantly strictured. Anorectal mucosa grossly normal. No mass noted. FNAB report was “Blood and granular debris. No malignant cells seen”.
The colorectal surgeon concluded that there is a complete clinical and pathologic response to the treatment. He did not recommend surgery. Instead, with the patient’s consent, chemotherapy was resumed. He scheduled another evaluation after her 12th chemotherapy. However, after the 11th cycle on August 2013, the patient refused to complete her next chemotherapy, thus the patient was sent back to the colorectal surgeon already.
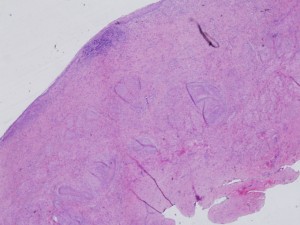
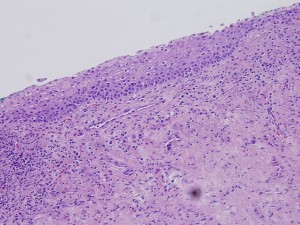
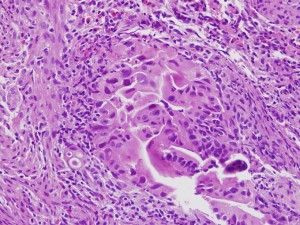
She was reevaluated by her colorectal surgeon under general anesthesia again on September 2013. Biopsies were done. The surface epithelium is generally unremarkable except for patchy areas of chronic inflammation. The underlying tissue is composed mostly a dense, fibrotic stroma. No evidence of malignancy is seen.
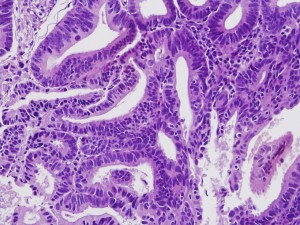
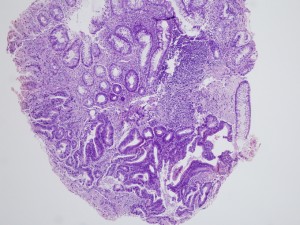
The pictures under the microscope are:
The advice of the colorectal surgeon was for the patient to have regular checkup. No operation is recommended at this time. As of August 2014 the patient is still doing very well, with no evidence of recurrence.
COLON CANCER IN A MALE PATIENT DISAPPEARED WHEN GENE THERAPY WAS ADDED TO STANDARD CHEMOTHERAPY
An 83 year old man was admitted in early August 2012. The colonoscope was inserted to 60 cm where it encountered a completely obstructing friable mass. Biopsy was done which showed intramucosal adenocarcinoma.
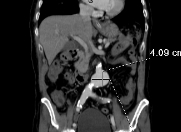
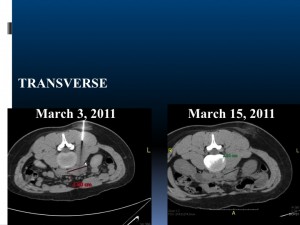
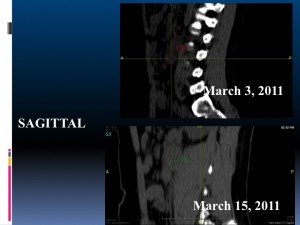
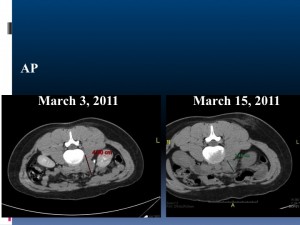
Abdominal CT scan without enteral contrast was also done which showed a thickened terminal ileum, cecum, ascending and transverse colon with maximum thickening of 1.2 cm, as well as saccular outpouchings in the ascending colon. No definite colonic mass was seen. And no evidence of metastasis. In addition, he was also found to have an aneurysm measuring 4.1 x 4.7 x 4.1 cm at the infrarenal aorta. He was seen by a vascular surgeon.
Operation was not done because the patient refused. He was also aware of the risk of aneurysmal rupture. Instead, we proceeded with Folfox chemotherapy in August 2012 and given every 2 weeks as outpatient thereafter for a total of 6 cycles. At the same time, Gendicine was given twice a week for 12 times.
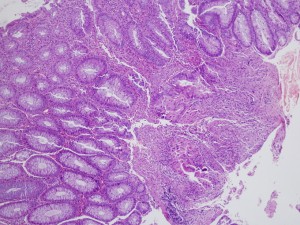
A repeat colonoscopy was done in October 2012. The scope was inserted up to 70 cm “where a circumferential mass was almost completely obstructing the lumen was noted. Attempts to pass the scope beyond the mass was unsuccessful. “ The biopsy report was “At least intramucosal adenocarcinoma. Comment: a more severe underlying lesion cannot be completely excluded.”
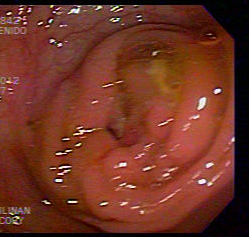
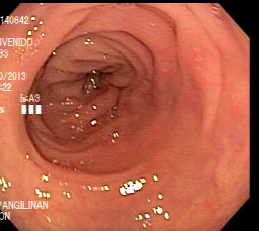
The colonoscopy findings:
The histopath of October 2013 showing intramucosal adenocarcinoma:
In November 2012, his treatment was changed to Irinotecan which was given every 3 weeks as outpatient. His last dose was in July 2013.
Another colonoscopy was done in August 2013. At this time, there was “note of spasticity at 70 cm and at the hepatic flexure. Further insertion done reaching up to the cecum with visualization of the appendiceal orifice… No gross mass lesion appreciated at the hepatic flexure.”
His latest checkup was in June 2014. There was no evidence of recurrence or metastasis at that time.
Wonders of Life
Mrs. Marlowe Ngo was diagnosed with metastatic cancer of the thymus. The thymus is an organ located in the front part of the chest. She lost her voice and had difficulty breathing. Her cancer was not operable. She did not get well with chemotherapy and radiation treatment. Her doctors told her she had 3 months to live.

According to Mrs. Ngo, “during my last treatment, that was December 24 (2011), my son asked my doctor if there was a chance for me to regain my voice. The doctor replied, ‘It is a 50-50 chance and if ever, it will take several months since vocal cord nerves had been damaged.’ Surprisingly after a month, I fully regained my voice as if nothing happened.”
Mrs. Ngo was able to go back to work and to travel outside the country after her gene therapy. It is now 17 months after her last p53 injection. Truly, miracles still happen.
Health & LIfestyle, August 2012 pp 28-29
13 year-old boy with rhabdoid tumor of the bladder
13 year-old boy with rhabdoid tumor (cancer) of the bladder underwent surgery (partial removal of bladder). He went to a well known hospital in China for further treatment. Chemotherapy drugs were injected directly to the tumor via the artery. Also given systemic chemotherapy and immunotherapy. After 2 months there was recurrence of tumor in the pelvis. Cryotherapy and brachytherapy were added to the treatment regimen but there was progression of the disease until it became stage 4. They came back to the Philippines and underwent p53 gene therapy plus another systemic chemotherapy. He received a total of 6 courses of induction chemotherapy and p53 gene therapy. The side effects were limited fever, some chills and headache which lasted a few hours only. His PET CT scan showed a marked decrease in the size of the pelvic mass with massive calcifications. On second look surgery, there were no more tumors seen in the pelvis. Another PET CT scan was done at the end of maintenance chemotherapy which did not show any abnormal uptake. So he is currently cancer free.
A 16 year-old boy who got well from Acute lymphocytic leukemia
A 16 year-old boy who got well from Acute lymphocytic leukemia 10 years ago and was already living a normal life comes back with multiple tumors in his paranasal area, neck, chest, abdomen and testicle. Biopsy of the excised testicle shows non Hodgkin lymphoma. He was given chemotherapy, monoclonal antibody and p53 gene therapy (Gendicine). The Gendicine was injected directly to the tumor in the abdomen. Some doses were given intravenously. He has now finished his treatment and is cancer free!
Gene Therapy success for 55 year-old woman with invasive ductal carcinoma
A 55 year old woman with invasive ductal carcinoma of the right breast underwent skin sparing mastectomy with TRAM reconstruction a year ago. The biopsy report showed a huge tumor around 9 cm in largest dimension with lymphovascular invasion and with seven out of 24 axillary lymph nodes positive for metastasis. She changed to a vegetarian diet and was very health conscious since then and she was apparently well until March of this year when she noted a mass above her right collar bone. A biopsy done showed metastatic carcinoma consistent with ductal primary. There was no evidence of other metastasis. This placed her at stage IIIC. She underwent chemotherapy but had to stop after 2 sessions because of severe side effects. She was also worried about the effects on the inferior vena cava filter that was placed because of previous history of deep vein thrombosis. At this point, she opted to undergo p53 gene therapy. She has completed 12 sessions of treatment and has been free of disease up to now.